Abstract
Introduction: Adults with AML have immune aberrations leading to immune suppression, exhaustion, evasion, and senescence. Early lymphocyte recovery (ELR) after induction TST is dominated by an expansion of oligoclonal peripherally derived regulatory T cells (Tregs). Pomalidomide (Pom), a small molecule immunomodulatory agent (IMiD), leads to the selective ubiquitination of Aiolos and Ikaros by cereblon; this ubiquitination increases IL-2 production, inhibits Tregs, and inhibits angiogenesis. We hypothesize that Pom administration after induction TST may enhance anti-leukemic activity through immune modulation.
Methods: A multicenter phase 1 dose escalation study was conducted to determine the safety and tolerability of Pom administration after induction TST in newly diagnosed AML and HR-MDS patients 18-65 years. Favorable-risk cytogenetics were excluded. All patients received induction TST with AcDVP16: Cytarabine 667 mg/m2/day continuous IV days 1-3, daunorubicin 45 mg/m2 IV days 1-3 (or idarubicin 8-12 mg/m2 IV days 1-3 in daunorubicin shortage), etoposide 400 mg/m2 IV days 8-10, followed by Pom administration at ELR (after day 14 and within 3 days of the total white blood cell (WBC) reaching ≥0.2x109/L above nadir, but no later than day 30). Pom dose escalation occurred in 2 cohorts: 10 days versus 21 days of administration, in a traditional 3+3 design.
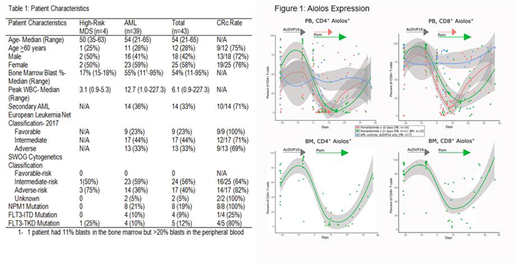
Results: A total of 51 patients were enrolled and 43 (AML: n=39, HR-MDS: n=4) received Pom across 3 institutions (Table 1). Eight patients did not receive Pom due to no ELR by day 30 (n=3), sepsis (n=3), noncompliance with treatment (n=1), and death prior to ELR due to acute respiratory distress syndrome (n=1). Median time for Pom initiation after AcDVP16 induction was day 21 (range: 15-30 days). Pom maximal tolerated dose (MTD) was 4 mg for 21 consecutive days at ELR. The most common non-hematologic grade ≥3 toxicities related to Pom were febrile neutropenia (30%), maculopapular rash (14%), and aminotransferase elevation (5%). Dose-limiting toxicities (DLTs) of Pom at 8 mg for 21 days were grade 3 ALT/AST elevation and grade 4 respiratory failure, respectively. Pom was discontinued early (median duration = 7 days; range: 3-20 days) in 14 (33%) patients due to disease progression (n=4), grade 3 rash (n=3), DLT (n=2), patient decision (n=2), progressive cytopenias (n=1), and grade 4 acute kidney injury (n=1).
Overall, 32/43 (74%) achieved CRc (CR: n= 30, CRi: n=2). Among the 4 HR-MDS patients, 2 (50%) achieved CRc, whereas 77% (30/39) of AML patients achieved CRc. Of the 32 CRc patients, 19 (59%) had no evidence of minimal residual disease (MRD) by standard testing (flow cytometry, FISH, cytogenetics, and/or molecular PCR). Encouraging CR rates were seen in poor-risk subsets: Age ≥60 years: 75% CRc (9/12); Secondary AML: 71% CRc (10/14); Adverse-risk cytogenetics: 82% CRc (14/17). Thirty- and 60-day mortality were 0 and 2%, respectively. Median time to neutrophil (≥1.0x109/L) and platelet (≥100x109/L) recovery was 38 (range: 28-86) and 33 days (range: 24-75), respectively. With a median follow-up of 23.9 months, median overall survival, disease-free survival and event-free survival were 33.8 months, 20.3 months, and 8.7 months, respectively.
Pharmacodynamic biomarker studies revealed a significant decrease in the expression of Aiolos in peripheral blood CD4+ and CD8+ T cells when compared with AML controls who received AcDVP16 induction but did not receive pomalidomide (p <0.05; Figure 1). Moreover, these findings were corroborated in the bone marrow where Aiolos expression in CD4+ and CD8+ T cells substantially decreased after pomalidomide initiation.
Conclusions: Pom can be added at the time of ELR after induction TST without increased toxicity and CR rates that compare favorably with historical controls of TST and other standard induction therapies. Despite administration at the time of profound cytopenias, Pom was well tolerated and did not significantly prolong hematologic recovery. Correlates suggest that Aiolos expression may be a pharmacodynamic biomarker of activity. Identification of immune biomarkers to predict for response and duration of response are ongoing. Further exploration of Pom both at the time of induction TST and during CR are warranted.
Zeidner:Rafael Pharmaceuticals: Other: Travel Fees; Merck: Research Funding; Asystbio Laboratories: Consultancy; Takeda: Other: Travel fees, Research Funding; Tolero: Honoraria, Other: Travel Fees, Research Funding; Celgene: Honoraria. Zeidan:Agios: Consultancy; Incyte: Employment; Novartis: Consultancy; Celgene: Consultancy; Ariad: Consultancy, Speakers Bureau; Gilead: Consultancy; Pfizer: Consultancy; Abbvie: Consultancy. Pratz:Astellas: Consultancy, Research Funding; Agios: Research Funding; Boston Scientific: Consultancy; AbbVie: Consultancy, Research Funding; Millenium/Takeda: Research Funding. Foster:Shire: Honoraria; Pfizer: Research Funding; Macrogenics: Research Funding; Celgene: Research Funding. Coombs:H3 Biomedicine: Honoraria; AROG: Other: Travel fees; DAVA Oncology: Honoraria; Abbvie: Consultancy; Incyte: Other: Travel fees. Luznik:WIndMIL Therapeutics: Equity Ownership, Patents & Royalties. Gojo:Amgen: Membership on an entity's Board of Directors or advisory committees; Jazz Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Merck inc: Research Funding; Amgen: Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal